Jeffrey Pollak, MD, has seen many incremental changes in medicine over the years, but rarely any game changers.
The Robert I. White, Jr. Professor of Radiology & Biomedical Imaging at Yale School of Medicine, (YSM) Pollak had a game-changing moment earlier this year while performing a minimally invasive procedure on a patient with life-threatening blood clots in his lungs.
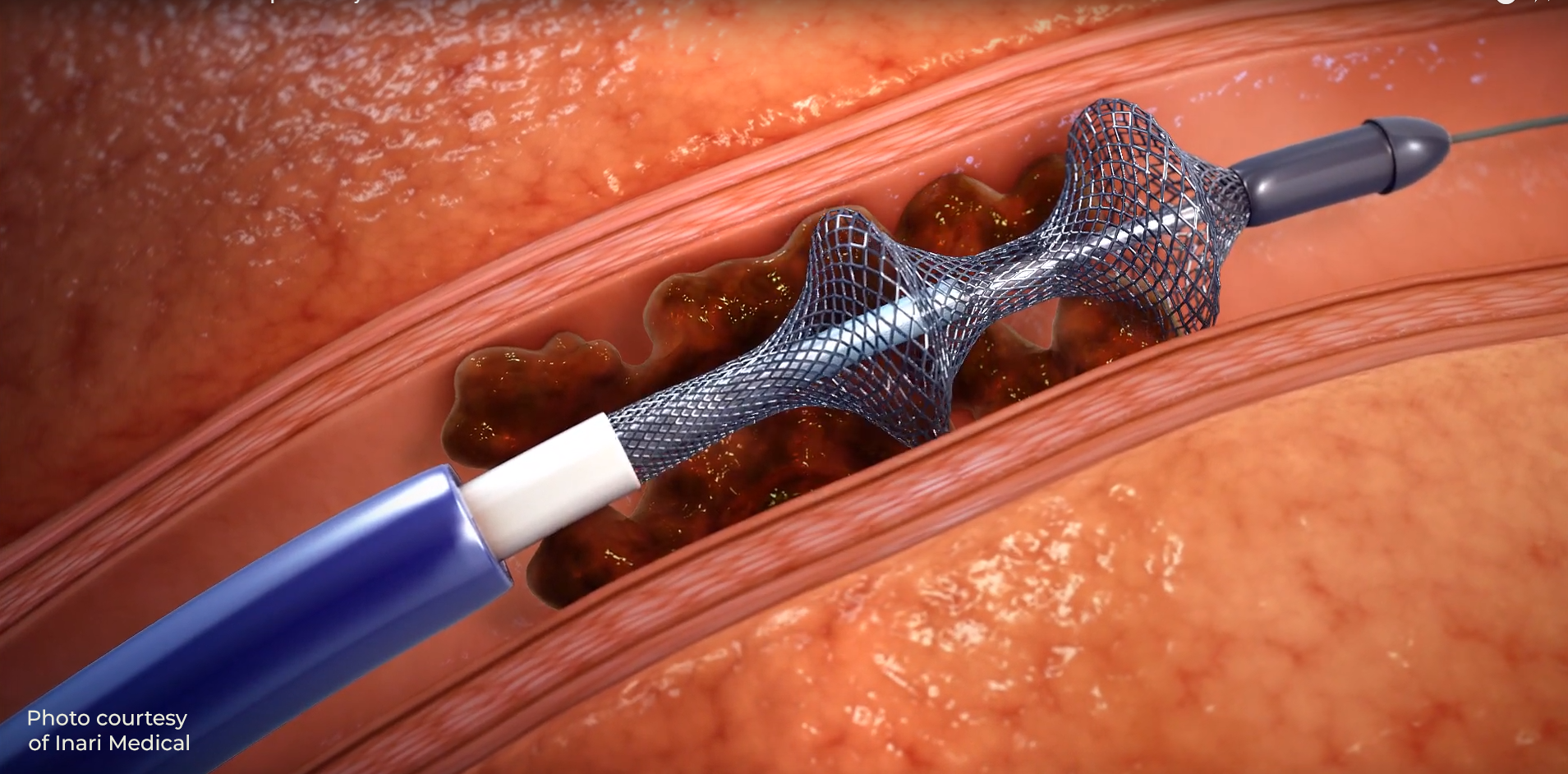
Through a tiny incision in the skin, Pollak guided a catheter into the pulmonary artery to the clots. As he retracted the catheter, he used a suction device to first pull the clots out of the artery and then out of the patient entirely through the skin incision.
“You could see the patient, who had been barely able to breathe, revive on the table as the clots were removed,” said Hamid Mojibian, MD, associate professor of Radiology & Biomedical Imaging at YSM who performed the interventional radiology (IR) procedure with Pollak.
“Such an immediate thrombectomy allowed the patient to turn the corner, right on the table, even before getting out to recovery,” said Kevin Kim, MD, professor of Radiology & Biomedical Imaging at YSM and the IR chief.
A main benefit of the IR procedure is that it does not require the use of thrombolytic agents –clot-busting medicines that can result in bleeding elsewhere in the body, said Pollak. “This expands our ability to treat older patients, or patients with other medical issues who are at a higher risk for bleeding,” he said.
Interventional radiologists at YSM are the first in Connecticut and among the first in the Northeast to successfully perform a pulmonary thrombectomy with the new mechanical device that does not require the use of the clot-dissolving drugs or a surgical incision into a blood vessel.
“With this new, innovative and successful treatment, we can treat our critical patients with a pulmonary embolism more safely and effectively, and save more lives,” Kim said.
Previously, a patient with a pulmonary embolism would spend six to 12 hours receiving thrombolytics with typically a one- to two-day intensive care unit stay. “If an embolism was life-threatening, the patient may require surgery to remove the clot,” Mojibian said.
“We can offer this treatment to our patients because of the collaborative work between radiologists, pulmonologists, hematologists, and the Yale New Haven Health team,” Mojibian said.
“We also have decades of experience in IR,” Pollak added. “So when a new procedure like this comes out, we are primed and ready to do it. We have the expertise to pick it up very quickly.
There are few things in medicine that are game changers. This is a quantum change in terms of what we can now do to treat our patients.
Jeffrey Pollak, MD
While other mechanical devices have been used to remove blood clots, they were not as effective and required the use of thrombolytics, although doctors used as little medicine as possible in those cases, Pollak said.
“When I saw the effect of this new procedure, my phrase was it is a game changer. There are few things in medicine that are game changers. Many things provide incremental changes, but these are quantum changes in terms of what we can now do to treat our patients,” Pollak added. A pulmonary embolism occurs when a clot breaks free from a vein and travels to the lung arteries. This can be a medical emergency, requiring quick intervention and treatment. Its symptoms – coughing, chest pain and shortness of breath – resemble many other medical conditions, including heart attack and pneumonia, so it can be difficult to diagnose. It is more likely to arise in people with certain medical conditions such as cancer or those with poor circulation. It is also associated with a sedentary lifestyle and long periods of inactivity, such as sitting during a long airplane ride. The people most at risk, however, are those with other medical issues, such as heart disease and cancer.